An introduction to building software for value-based care
I attended a talk on ‘The future of the EHR’ and was disappointed. The capabilities I saw drive great care for patients at Cityblock were nowhere to be seen in the ‘EHR of the future’. At Cityblock, our ideal electronic health record (EHR) looked like a customer relationship management (CRM) tool with a side of EHR. Given the gap, I wanted to look back at my journey as the first engineer and head of engineering for Cityblock Health. What did we do that mattered and why?
Our aim at Cityblock was to improve the lives of of people in underserved communities. However, our engineering and product team was mostly people from non-healthcare backgrounds with some wild ideas for what would best help our staff. Some ideas were voice/dictation, radically simplifying tasks/collaboration, a command line and automating care plan management but our most successful projects were relatively small builds; things like:
- UI, policies and procedures for care workers to text patients
- Realtime integrations with health information exchanges (HIE) that drove immediate in person interventions, mainly around hospital admissions
- Spreadsheet import/exports for matching providers and patients and rebalancing care teams
Why did those ‘features’ matter, and so many didn’t? Let’s go back to what value-based care is all about.
Value #based care
Value-based care is about putting patients first in everything that we do - that is the singular core value. The patient is our customer and our full focus is providing a great service to our customers over the long term.
However, I and my teams built software; we don’t actually directly see patients. How do we…’put patients first’?
We put patients first by helping help care workers implement the right interventions. We orchestrate - appropriate people, appropriate place, appropriate information, appropriate time.

What is value-based care?
Value-based care (VBC) is a new-ish approach to paying for healthcare. It generally means that medical professionals take on financial responsibility or ‘risk’ for the quality of the care they provide. This is very different from FFS ‘fee for service’ where providers focus on doing a discrete task well. In FFS, providers have a reputation to manage but they get paid the same regardless of readmissions or complications in the care they provide — they also do not look far outside of the medical scope to issues like transportation, housing or mental health.
There may be more value-based care financial models than Pokemon. Most of the time they take the form of combining many services into one ‘bundled payment’ (like combining prep, surgery and followups for a knee replacement), shared savings, or partial and then full risk (sometimes called 'capitation’). Risk approaches are unique since the company can lose money if the costs for a patient outpaces their estimate. When calculating cost in a risk agreement, medical providers and insurance companies debate about whether to include the costs of physician, specialists, emergency visits and pharmacy.
One issue with shared savings and risk contracts is that they incentivise the providers to lower costs - which could mean they (illegally) deny or discourage services in the short term to save on cost. To counteract that incentive, most value-based contracts are for 3+ years and so would penalize such behavior if it increased cost down the line. In practice, most value-based care providers focus on reducing utilization of the emergency room in favor of more frequent and longer primary care or social needs focused visits. An ED admit costs about $2200 in NYC and those dollars could pay for many hours of in home specialized services.
Why not fee for service?
A relatively healthy and wonderful person we cared for at Cityblock averaged 15-20 emergency visits per month (1 every other day!) and had not seen a primary care doctor in many years. On the other end of the utilization spectrum, I recently booked an appointment with my primary care doctor and the next available appointment was 3 months out. The day of the visit I took about two hours off work to see the doctor for about 8 minutes and pay them a $75 copay.
Most folks reading this may not go to the emergency room very frequently, but many relatively healthy people do. The ER is functionally an as needed free medical service. People who may not be able to take 2 hours off work, make an appointment months out and afford a co-pay rationally use the ER when they need medical attention or are just worried about a medical issue.
Value-based care is an attempt to better meet peoples needs and align incentives between people receiving care, providers and the insurance companies. I believe that is best served by providers creating deep relationships with their patients and acting proactively rather than reactively.
The value journey
VBC tools support a few key stages of the patient-company relationship. In the simplest terms, a provider reaches out to patients, they actively listen to the patient and then they help the patient reach their goals. The steps might be:
- Outreach: How can we find and start a conversation with our patients?
- Knowledge and trust building: How can we learn more about the real challenges this patient is facing? How can we deepen our relationship so there is two-way listening?
- Population management: What interventions can I do today that will reduce the chance of interventions later? What is the most important intervention for the person who needs it the most?
A patient will move between each of these three areas of focus but sometimes they change stages in reverse such as if a first visit does not go well, the provider may try another approach to build trust.
The people doing the work
I find it helpful to learn about the people caring for patients and their jobs before thinking about the tech. People first.
A big insight of value-based care model is that complex care management requires establishing a trusted contact with the patient that is separate from an individual medical or behavioral specialist. A trusted non-medical contact can provide long, rich visits and higher quality care at lower cost through being the ‘quarterback’ of a broad team of experts.
The ‘quarterback’ of the care team (group of people cooperating to care for an individual patient) can be a community member who manages the relationship with the patient. They provide trusted referrals to and seek guidance from a team of specialists and a network of community organizations. Those specialists may be on a care team that meets daily. The medical and social needs specialists may co-lead a daily care team meeting or ‘huddle’, but on a patient level, they are usually pulled in to solve specific issue and/or co-craft a forward looking care plan by the ‘quarterback’.
In terms of relative scale, the ‘quarterback’ may focus on ~20 patients and a specialist like a social worker may see ~100 (NOTE: lots of variance here - sometimes the quarterback may see 100+).
Brief descriptions:
Community health partner / Quarterback
- Foster lasting relationships as the face of the team and key point-of-contact.
- Help the patient in achieving their goals, identifying new needs, and coordinating care.
- Cooperatively manage care for a population living with complex medical and behavioral health needs.
NP/PA, RN and PCP (NOTE: very different roles - but all focused on medical operations)
- Co-manage a panel of complex patients in a value-based care environment
- PA/NP: Provide comprehensive care management, chronic disease management, urgent home-based and community-based primary care visits, preventative care and wellness. Work with relevant other providers around behavioral health and other specialities.
- PCP: Diagnosis, treatment, counseling, medication management, acute triage and follow up care.
Social worker / Behavioral health / LCSW
- Coordinate a treatment plan, perform psychotherapy, support medication management…
Other folks could include lawyers, transportation specialists, benefits specialists and much more.
Outside of a care team, there are broader management roles like Medical directors, practice management, care management who are looking across many care teams to ensure quality, compliance and a consistent care model across care teams. On the business side, there are market operations folks that look at whole geographic areas and think strategically about number of staff, patients, community partnerships and physical resources like clinics or equipment.
Tech fluency of staff
We have looked briefly at their roles and responsibilities but these folks are used to a very different set of tools than a person who sits in an office (…home office) all day. It terms of tech experience generally safe to assume people:
- are good at using lots of different complicated tools and finding workarounds
- don’t like using iPads for work (attention…every digital health startup)
- share tips and tricks with each other verbally
- have never used Slack / Teams / Discord
- have never used GSuite for documents or calendar (most medical folks have an office admin manage their calendar)
- are comfortable with email but have different norms
- are comfortable with texting or messaging apps
The role of tech
The role of tech is to put the patient first. Tech teams in this world need to rigorously manage resources and focus in order to provide care across the many dimensions and cover seemingly endless edgecases. Tech teams also need to help the overall business iterate quickly toward a model that is proven to work.
I’ll talk more about the vast set of functionality in a future post but generally the needs of the business far outstrip the capabilities of the team at least initially. This means there are lots of discussions around build vs buy vs integrate vs outsource.
In general, you want to build things that are unique to the company and core to the model - that is where you will want to iterate the most. Everything else can be outsourced, bought or partnered to get but if you can’t find a partner that meets your quality and speed bar, it may make sense to bring that area in house as well.
Here is a little chart:
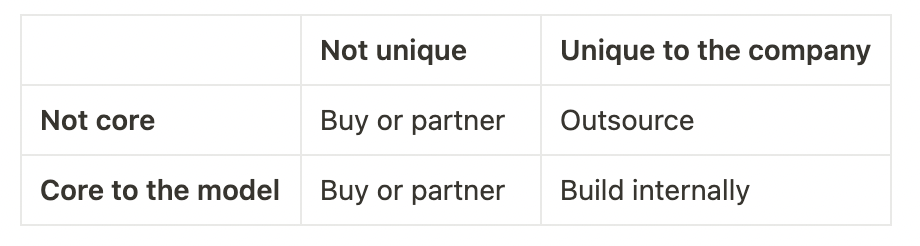
In software design, I talk a lot about ‘optimizing for flexibility’ and building software that is easy to safely modify. Ease of modification is far more important than the speed of the code. The reality of running a business is that things change. Business areas that were not core become core and areas that were unique may get less unique as the competitive (and political!) landscape changes.
While tech teams do need to creatively services all business needs, the area of focus for in house teams should be areas that are both unique and core, or else your focus will be spread far too thin to provide differential value and real innovation.
Those ‘unique and core’ tools may be:
- tools for selecting, prioritizing and matchmaking patients
- the tool(s) providers use in the field
- tools that management roles use to make informed market level decisions
Areas that are core but less unique might be
- Identifying quality gaps
- scheduling - however the quality of external tools may not be high enough
Areas that are not core but unique might be
- reports for external partners
The future of value-based care tools
VBC asks providers to do A LOT. Providers desperately need new tools in this world.
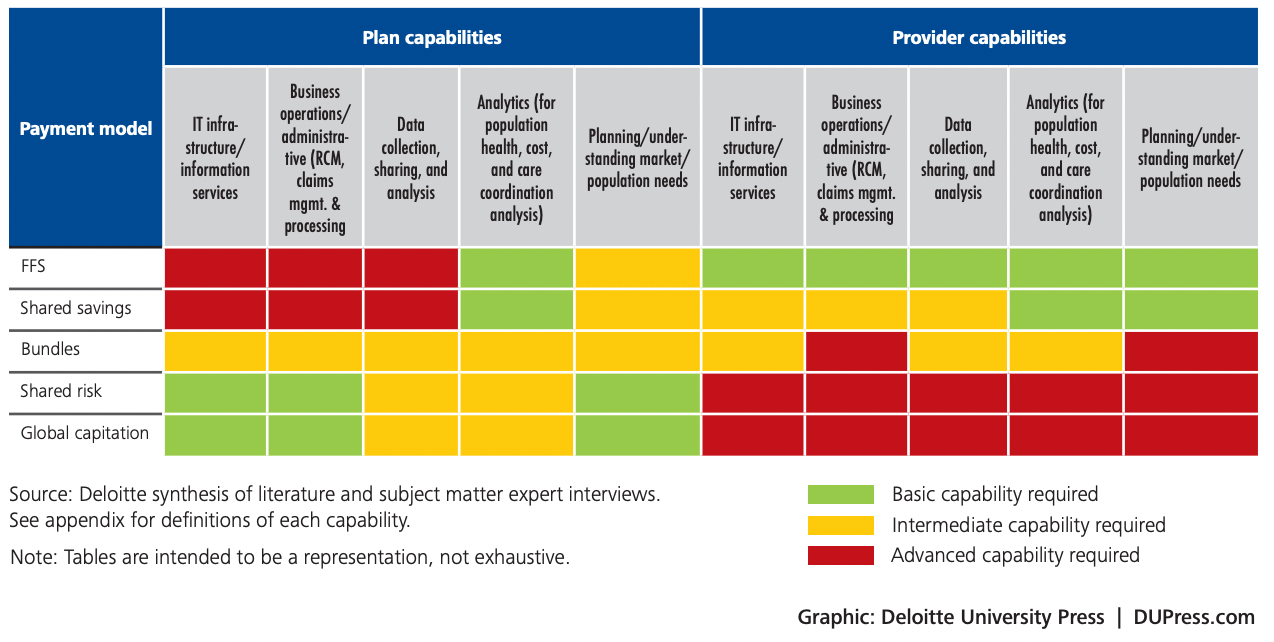
I believe future of EHRs is going to be a bifurcation around teams concerned with volume and teams concerned with value. This story is told in the above chart where providers taking on risk need more tooling around data collection, analysis and planning than providers handling FFS.
In addition to doing their job well, value focused teams need to think about the future, and actively seek out patients (rather than waiting for them to schedule). Value-based cares tools should help care teams manage relationships with their patients and think ahead to help maintain trust and reduce the risk of undesirable outcomes.
If you squint, this starts to look a lot like high powered CRM - like a Zendesk or Salesforce and less like a traditional EHR.